Ogedegbe G, Teresi JA, Williams SK, Ogunlade A, Izeogu C, Eimicke JP, Kong J, Silver SA, Williams O, Valsamis H, Law S, Levine SR, Waddy SP, Spruill TM. Home Blood Pressure Telemonitoring and Nurse Case Management in Black and Hispanic Patients With Stroke: A Randomized Clinical Trial. JAMA. 2024 Jul 2;332(1):41-50. doi: 10.1001/jama.2024.6609. PMID: 38842799; PMCID: PMC11157441.
Dr. Confounder previously wrote about a series of studies on the impact of nighttime antihypertensive dosing, and how this allows us to observe the clinical effect of reducing blood pressure without changing overall medication exposure. In these studies, no difference in major adverse cardiac events was identified. Another way to look at this is by studying the effect on blood pressures and adverse outcomes that comes with better adherence. Again, the benefit of such a study is that ideally the regimen is not significantly changed, thus removing the confounding pleiotropic effects from the equation.
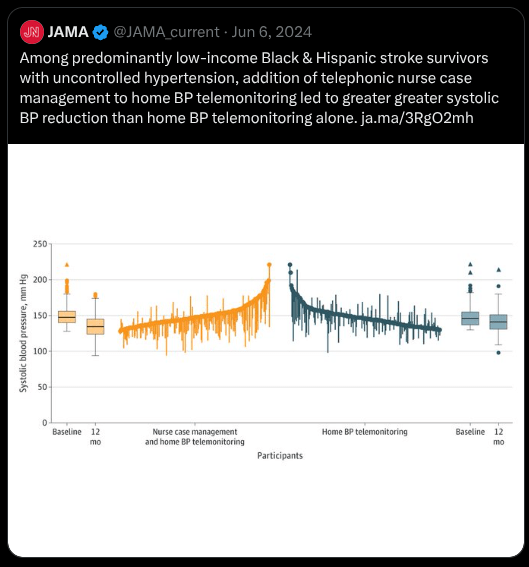
A study published in JAMA in 2024 (https://jamanetwork.com/journals/jama/fullarticle/2819467) did just that. A cohort of 450 low income Black and Hispanic stroke survivors were randomized to receive either home blood pressure telemonitoring (HBPTM) and nurse case management (NCM) phone-based follow-up or HBPTM alone.
After 12 months, the patients receiving both interventions saw significantly greater blood pressure reductions, approximately 10 mmHg more than the HBPTM group (−15.1 mm Hg vs. −5.8 mm Hg). Despite this, at 24 months, the rate of recurrent stroke was almost exactly the same (4.0% in both groups).
A JAMA publicity tweet conveniently left out this second part.
As always, even in this high risk population, or especially in this high risk population, large blood pressure reductions on their own fail to demonstrate superior outcomes.
More evidence for the confounding that is almost always present when better outcomes are attributed to intensive blood pressure control.
Leave a comment