Guo X, Sun G, Xu Y, Zhou S, Song Q, Li Y, Ouyang N, Li G, Cheng Z, Ye N, Wang J, Zhou Y, Yang H, Shi C, Wang C, Liu S, Zhu W, Moran AE, Ning G, Bi Y, Wang W, Cai J, Li J, Sun Y; BPRULE Study Group. Benefit-harm trade-offs of intensive blood pressure control versus standard blood pressure control on cardiovascular and renal outcomes: an individual participant data analysis of randomised controlled trials. Lancet. 2025 Sep 6;406(10507):1009-1019. doi: 10.1016/S0140-6736(25)01391-1. Epub 2025 Aug 31. PMID: 40902616.
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(25)01391-1/fulltext
Disclaimer: I am aware that primum non nocere is not actually a part of the Hippocratic Oath, and it is an almost completely useless principle in clinical practice.
Following SPRINT and a number of other recent randomized trials comparing different blood pressure thresholds, a metanalysis was published in September in The Lancet, exploring net benefit of intensive blood pressure treatment.
In a combined cohort of more than 80,000 patients over about 3 years, they showed a 1.73% absolute reduction of risk of cardiovascular events and a 1.82% absolute risk increase in relevant adverse events. But as always, the complexity of blood pressure treatment was reduced to “antihypertensive medications.”

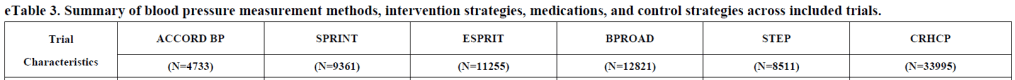
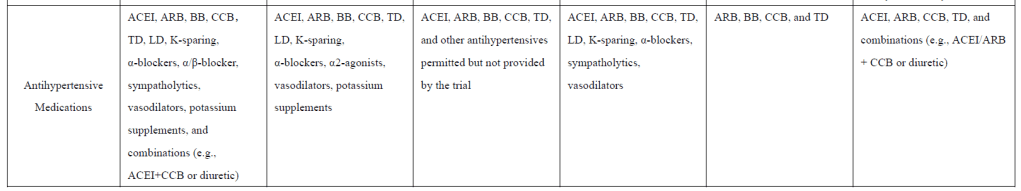
(Supplemental materials p. 46)
As always, patients with more room for blood pressure suppression stand to accrue many non-blood pressure risks and benefits from higher doses of specifically cardioprotective and renoprotective drugs.
It is also worth considering one of the subgroup analyses, in which the net benefit of intensive treatment was greater in patients without chronic kidney disease. This is counterintuitive: Considering that a primary reason to treat CKD is that it is a huge risk factor for cardiovascular disease, one would think that patients with a disease for which blood pressure reduction is standard of care would stand to benefit more than patients without that disease.
One possible explanation is that patients with CKD didn’t accrue the same level of cardiovascular benefit because the medications carrying more cardiovascular benefit were contraindicated due to the patients’ renal dysfunction. In other words, the benefit of this treatment may manifest in something other than systolic blood pressure.
Nonetheless in an NEJM Journal Watch review of this study, the reviewer stresses the importance of intensive blood pressure control “in my highest-risk patients” (such as those in subgroups shown to accrue less net benefit from such treatment).
Leave a comment